Videos
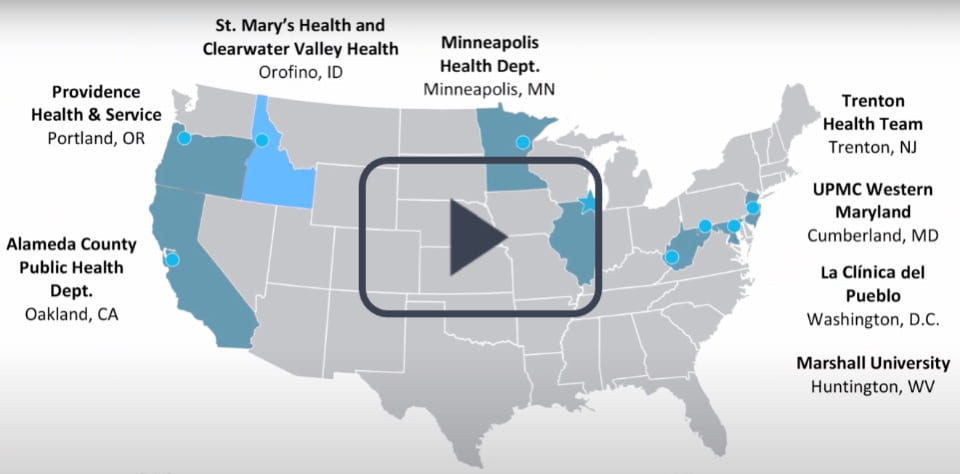
The Bridging the Gap: Reducing Disparities in Diabetes Care initiative was a 5-year project funded by the Merck Foundation that aimed to improve access to high-quality diabetes care and reduce health disparities for patients living with diabetes. In this video, we provide three key takeaways from our initiative on how we can improve diabetes care and reduce health disparities.
Bridging the Gap in Diabetes Care
Bridging the Gap: Reducing Disparities in Diabetes Care is a 5-year initiative funded by the Merck Foundation that seeks to improve access to high-quality diabetes care and reduce disparities in health outcomes among vulnerable and underserved populations with type 2 diabetes in the United States. Bridging the Gap grantees aim to build sustainable partnerships to address the medical and social factors that influence health, redesign health care systems to improve diabetes care, and improve health outcomes and decrease disparities for individuals and communities with type 2 diabetes.
Bridging the Gap—Reducing Disparities in Diabetes Care: Cross sector Partnerships to address SDOH
Reducing disparities in healthcare delivery is only a partial solution to resolving disparities in health outcomes disproportionately experienced by marginalized populations. Healthcare systems have increasingly recognized the importance of addressing the social determinants of health (e.g. food insecurity, employment, housing, language barriers, legal needs) to eliminating such disparities. Addressing both medical and social needs of patients requires cross-sector partnerships between healthcare systems and non-healthcare sectors. This panel-style symposium will focus on the National Program Office of Bridging the Gap (BTG): Reducing Disparities in Diabetes Care and three BTG grantees, representing unique health care organizations working to create complex care ecosystems by developing synergistic partnerships with community organizations. Panelists will discuss their partnerships with non-healthcare organizations and the factors that support alignment as they work together to meet both the medical and social needs of a shared population.
This presentation was presented online at the 2020 Society for General Internal Medicine (SGIM) annual meeting and is shared with support from SGIM and Bridging the Gap: Reducing Disparities in Diabetes Care.
Bridging the Gap in Oakland, CA
Alameda County Public Health Department partners with local clinics to improve diabetes care by supporting peer-led diabetes education and expanding programs that provide physical activity opportunities in the community. A local clinic, Roots Community Health Center, bridges gaps between medical and social care systems through peer navigators, who provide case management for health conditions and address social needs (e.g., employment) that impact the health and well-being of their clients.
Check out Alameda County Public Health Department and their clinical partner website here:
http://www.acphd.org/
https://rootsclinic.org/
https://www.tvhc.org/
Bridging the Gap in Washington, DC
At La Clínica del Pueblo (LCDP), health educators help Latino immigrant patients navigate comprehensive health services and community resources in Washington DC and Maryland communities. LCDP offers a safe space where care teams can bridge vital gaps in diabetes care including food insecurity and legal barriers. LCDP provides linguistically and culturally appropriate health and education services and acts as a community hub and anchor in the communities it serves.
Check out La Clínica’s del Pueblo’s website here: https://www.lcdp.org/
Bridging the Gap in Portland, OR
Providence Health & Services bridges gaps in care for patients with diabetes by partnering with a local organization, Impact NW, and co-locating a community resource desk at three Portland, Oregon family medicine clinics. A community resource desk is staffed by resource specialists from ImpactNW who have extensive knowledge of and experience with the social services sector. As part of a broader health system effort to reduce gaps in care and integrate medical and social services for patients, the community resource desk provides a timely and accessible resource to address unmet social needs.
Check out Providence-Oregon’s website here: https://oregon.providence.org/
And ImpactNW’s website here: https://impactnw.org/
Bridging the Gap in Huntington, WV
Mountain Comprehensive Health Corporation (MCHC) bridges gaps in diabetes care by overcoming healthcare access barriers in rural areas of Kentucky. Community health workers at MCHC address social needs by engaging with high-risk patients and collaborating with community-based programs including farmers markets, transportation assistance and home gardening.
Check out MCHC’s and their grantee partner, Marshall University, here:
https://www.mchcky.com/
https://www.marshall.edu/
Bridging the Gap in Orofino, Idaho
St Mary’s and Clearwater Valley Hospital and Clinics (SMH-CVHC) bridges the gap between community and clinical outreach in remote areas by coordinating unique solutions with community partners. Across three frontier counties in north central Idaho, community health workers engage patients and community residents through community events and by working closely with local food distribution sites. The community health workers offer health information and resources to patients with diabetes and options to connect them to the health care system.
Check out our Bridging the Gap website to learn more: http://bridgingthegapdiabetes.org/
Also, check out SMH-CVHC’s website here: https://smh-cvh.org/
Bridging the Gap in Trenton, NJ
Trenton Health Team is an innovative, multi-sector partnership that convenes clinical and community-based organizations from diverse sectors. Trenton Health Team draws upon community feedback to engineer care pathways and processes that bring solutions to community-based organizations and clinical teams, prioritizing strategies to improve both individual and population health. From peer-led diabetes education to community forums to tools that support frontline providers and staff in the clinic, Trenton Health Team and their partners bridge the gap in diabetes care across the city of Trenton.
Check out Trenton Health Team’s and their partners websites here: https://trentonhealthteam.org/
https://www.capitalhealth.org/
https://henryjaustin.org/
https://www.stfrancismedical.org/
Bridging the Gap in Cumberland, MD
UPMC Western Maryland (UPMC-WM) bridges gaps in care for patients with diabetes by embedding healthcare services at community events and connecting patients with chronic conditions to a multi-disciplinary care team. The care team identifies and addresses medical and social needs, and patients receive individualized support to improve self-management and health outcomes. UPMC-WM relies on strong connections with their community as they foster relationships between their patients and the clinicians/staff who serve them.
Check out UPMC-WM’s website here: https://www.wmhs.com/
Bridging the Gap in Minneapolis, MN
Social needs can directly impact a patient’s ability to manage chronic conditions like diabetes. It takes a comprehensive strategy and alignment of resources in clinics and communities to address these social needs. The Minneapolis Health Department (MHD) and three federally qualified health centers (FQHCs), Neighborhood HealthSource, Native American Community Clinic, and Southside Community Health Services have developed systems that support patients within and outside of the clinic. These FQHCs bridge gaps in care and support the medical and social needs of patients with diabetes by integrating certified diabetes educators and community health workers.
Check out MHD’s website and their clinical partners here:
http://www.minneapolismn.gov/health/
https://neighborhoodhealthsource.org/
https://nacc-healthcare.org/
https://www.southsidechs.org/
Y4 Annual Meeting, Part 1: Screening & Referral Workflows
UPMC Western Maryland (UPMC-WM) bridges gaps in care for patients with diabetes by embedding healthcare services at community events and connecting patients with chronic conditions to a multi-disciplinary care team. The care team identifies and addresses medical and social needs, and patients receive individualized support to improve self-management and health outcomes. UPMC-WM relies on strong connections with their community as they foster relationships between their patients and the clinicians/staff who serve them.
Check out UPMC-WM’s website here: https://www.wmhs.com/

Copyright © 2021 — The University of Chicago