Stories from the Field: Oscar Flores
Hi Oscar, please tell us a little about yourself.
My name is Oscar Flores, I’m a Behavioral Health Therapist and a Clinical Social Worker by training. I have been at La Clínica del Pueblo for over six years. La Clínica del Pueblo is a community health organization, based in Washington D. C. It was created by immigrants to serve people who had been displaced from their home countries due to political instability, poverty, and war. Many of our patients immigrated to this area during the civil war in El Salvador between the 1970s and 80s. Our approach to diabetes care is holistic team-based care. Because of our patient population, many don’t speak English, and many are underinsured or have no insurance at all. Some deal with other social determinants of health, such as poverty, very limited access to healthy foods, ongoing stress, and prolonged history of trauma which we see a lot with our patients. So we have a whole hosts of social determines, and psychological social determinants of health. That’s why our care team is composed in a way that we can assess our patients in different areas of need that directly impacts their health
What are some key factors in your community that impact patients’ health, especially for Lantix immigrant patients living with diabetes?
Place matters. Every geriatrician and community is different. In our patient population, we do have safety nets. In Washington D.C. we have the D.C. alliance that offers access to primary care and medication. But there is no access to behavioral health which is a barrier.
What have you learned from working in partnership with other organizations in your community? How are you working together to improve health?
Because we have limited resources in a community that is complex with multiple needs and barriers. At La Clínica del Pueblo we cannot do everything by ourselves so we rely heavily on our partnership in our community health program. La Clínica del Pueblo’s main role is to make bridges with other community partners so that way we can support our patient’s access to food and legal aid. Some of our patients have an immigration status that places a big role in their wellness. It’s very difficult to stabilize someone who has chronic stress when the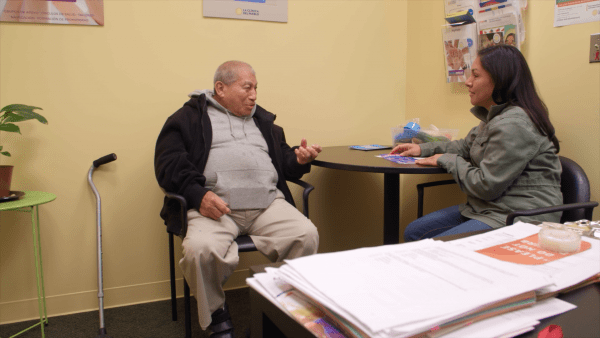 stress is still going on. That is why I depend heavily on our care coordinators for referrals for immigration, access to food, and access to medication. We have some patients who do not have insurance we have to find other ways to access their medication. Although these pieces all fit together our aim at La Clínica del Pueblo is to provide all the resources that our patients need so we can see better outcomes in their health. Health outcomes are not dependent on the dioecious they are also dependent on the patient’s environment and their access or lack of access to resources.
stress is still going on. That is why I depend heavily on our care coordinators for referrals for immigration, access to food, and access to medication. We have some patients who do not have insurance we have to find other ways to access their medication. Although these pieces all fit together our aim at La Clínica del Pueblo is to provide all the resources that our patients need so we can see better outcomes in their health. Health outcomes are not dependent on the dioecious they are also dependent on the patient’s environment and their access or lack of access to resources.
How has COVID-19 changed your work in diabetes care?
When COVID-19 started almost two years ago now. It was a big change. I have been a clinical social worker for seven years I have never imagined what came after COVID-19. It was a big change in how we delivered the care we had to modify operations. We were all moved (from the office) to a work-from-home environment. But we continued to make sure that our patients were connected to us and our services. Before COVID-19 we already had a telemental health program. So for the behavioral health team, it was an easier transition because it was already part of the program. COVID-19 affected our workflow because we were not in the same space so our coordination and collaboration ended up being challenging. We had to develop new protocols and procedures to make sure that we preserve our essence which is team-based collaboration and coordination.
Are there any lessons from the pandemic we should continue forward in diabetes care?
During COVID-19 not only did we see the horrors of the pandemic we saw the cracks in the healthcare system. In general; who has access to what? Because of their immigration status, many of our patients didn’t have financial relief as many Americas did. I would say a majority of our patients did not receive a stimulus check. Many of our patients were affected directly because they are essential workers and still had to show up to work. We are trying to lessen the barriers and impact on our community; during COVID-19 all the issues became magnified.
Many of our patients were affected directly because they are essential workers and still had to show up to work. We are trying to lessen the barriers and impact on our community; during COVID-19 all the issues became magnified.
