Hello, please introduce yourself and describe your position at La Clínica Del Pueblo.
My name is Rodrigo Stein, and I’m the Director of Health Equity and Strategic community Partnerships at La Clínica Del Pueblo, the Department of Health Equity and Strategic community Partnerships has two major functions, reducing barriers associated with the social determinants associated with immigration as a social determinant of health, and reducing the barriers for medical care relating to language barriers. We facilitate medical interpretation services for patients needing specialty care.
How is La Clínica Del Pueblo’s approach to diabetes care different from what patients may experience in other health care facilities?
La Clínica consistently has promoted the idea that immigration is a social determinate of health, and as such, It requires a multi-layer approach to address this, including how we approach diabetes care. Because immigration status affects a person’s abilities to gain meaningful employment. It affects a person’s ability, to obtain health insurance, whether that’s employer-sponsored or publicly subsidized health care. La Clínica’s approach recognizes these barriers and works to address them by strengthening multisectoral partnerships that address the barriers that are visible and tangible with immigration. Such as facilitating food access, facilitating referrals for legal organizations, addressing and minimizing some of the barriers associated with immigration as well as this network of medical interpretation when engaging with specialty care.
Such as facilitating food access, facilitating referrals for legal organizations, addressing and minimizing some of the barriers associated with immigration as well as this network of medical interpretation when engaging with specialty care.
As the Director of Health Equity and Strategic Community Partnerships, how does your role support diabetes care to address both medical and social needs?
My primary function is to strengthen those intersectoral partnerships. Whether it’s legal food access, so they understand the barriers that some of our community faces, whether that’s a partner, having language access services on-site, or facilitating interpretation service specifically when we speak about the legal issues. Through our food access partners that they understand that not all of our community will be eligible for Snap or Witk benefits due to their immigration status. These partnerships have to be mindful of these barriers and we have to create joint solutions.
How has COVID-19 changed your work in diabetes care?
I believe that one of the ways at COVID transformed the organization was by developing more intentional protocols and processes of how to be able to do remote work. For example, I know, that the diabetes management classes, were all done in person. A transition from facilitating six weeks to eight-week behavior change classes, over zoom or existing remote technologies required a lot of protocol development, also a lot of training on behalf of patients, a lot of our patients are older and limited English proficiency. A lot of these technologies unfortunately are not easy to just stop by and explain in simple language in Spanish. It took a lot of effort from the health educators to explain to people how to facilitate the available internet tools. In the early stages of COVID-19, we did the transition for La Clínica to become a food distribution hub something that was never done before. So we recognize the immediate material need, and thanks to strong partners and a strong network of food assistant partners, La Clínica absorbed the responsibility in the early stages of the pandemic becoming a full distribution site specifically for patients at risk or living with diabetes.
Are there lessons or changes from the pandemic that we should carry forward in diabetes care?
For immigrant communities, if jurisdictions don’t recognize or don’t allow for public-funded options or exclusion through the type of employment that have access to insurance. I think organizations that work with immigrant communities should be on the policy front, examining what options exist at the county or state level to guarantee access to care. On the other front, partnership building and addressing the immediate and material social needs, such as food, but not only any type of food, healthy and culturally appropriate food that recognizes the community, is also an important step. And from that social need build the case that will be addressed immediately.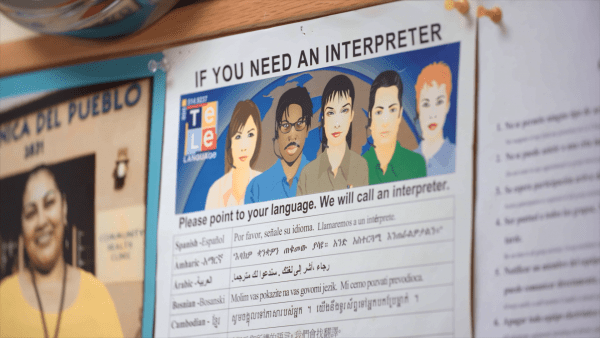 That is not a long-term system solution. So, what policy changes have to have to change, or at that bigger level, we’re talking about wages, we’re talking about worker protections, were talking about long-term immigration reform. That has two for the Latino community, especially the immigrant Latino community, and more specifically Low-income Latino community in an immigrant community. Those are the systemic changes that need to be pursued.
That is not a long-term system solution. So, what policy changes have to have to change, or at that bigger level, we’re talking about wages, we’re talking about worker protections, were talking about long-term immigration reform. That has two for the Latino community, especially the immigrant Latino community, and more specifically Low-income Latino community in an immigrant community. Those are the systemic changes that need to be pursued.
To continue supporting medical and social needs for Latino/a/x patients living with diabetes, what are some of your advocacy priorities in your region?
We’ve been successful to eliminate one of the barriers for the D.C Alliance. We’ve been able to successfully push, a recertification period to a year matching the Medicaid recertification process. However, that is still incomplete. Even though, though we are very grateful for the effort and our partner Coalitions Work. The alliance is still not comparable to Medicaid, since it doesn’t cover services such as mental health. I know when we speak about health, we define it as the complete social mental, and physical sense of well-being, not only a physiological. Integrating mental health will be very important as the next step for our advocacy with the D.C Alliance. Because we are in multiple jurisdictions, not only in the District of Columbia, we work in Prince George’s county in Maryland, seeking county or state solutions within the state of Maryland, that can increase access to high-quality and culturally appropriate health care for the immigrant community. Whether that is pursuing unique county funding to create a similar insurance program such as the alliance, or whether that’s going at the state level.
