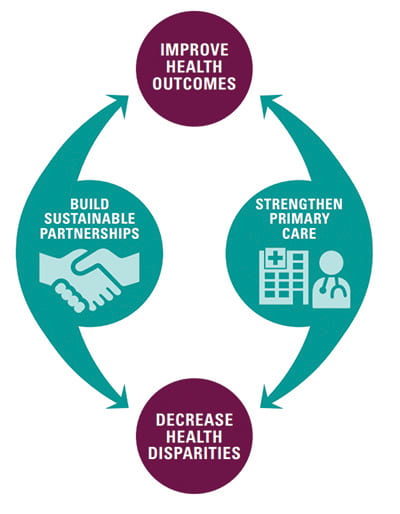
We are delighted to launch Bridging the Gap, a pioneering effort to reduce diabetes disparities by addressing the social and medical causes of such disparities in eight communities around the country. We seek to transform primary care, build partnerships between health care and social services/community resources, and generate evidence for sustainable models that address the medical and social needs of vulnerable populations. Despite diabetes being a priority condition for many health care organizations, policymakers, and patient groups, disparities in quality of care and patient outcomes have persisted across race, ethnicity, and socioeconomic status. Diabetes is often viewed as the model disease for addressing chronic care, as efforts to achieve optimal outcomes require effective patient self-management, the right care by clinicians, and opportunities for patients to engage in healthy eating and physical activity in their daily lives. Moreover, social determinants of health (SDOH), such as access to healthy food, stable housing, safe neighborhoods, affordable transportation, and livable wages, are important drivers of diabetes outcomes. In fact, the American Diabetes Association has identified addressing SDOH as a key issue and is currently performing a scientific review of the literature about how SDOH affect patient outcomes and what interventions can improve those outcomes.
Our eight grantees are diverse and at the forefront of innovative solutions to improve diabetes outcomes for high-risk patients. These grantees range from health departments in Alameda County and Minneapolis, a federally-qualified health center serving Hispanic patients in Washington, D.C., rural providers in West Virginia and the Appalachian region of Maryland, a frontier clinic in Idaho, to urban providers in Trenton, New Jersey, and Portland, Oregon. These providers care for racially and ethnically diverse populations, including African-American, American Indian/Alaska Native, Latino, and low-income white patients. Our grantees represent a range of insurance types (e.g., uninsured, Medicaid, private insurance) and payment types (e.g., managed care, fee-for-service). Thus, we have diversity in terms of geography, healthcare organizations, patient populations, and payer mix, among the grantees.
All eight grantees are testing different ways to organize their system of delivering care, provide tailored education and services to their patients, partner with community agencies to address SDOH, and create the business case to support sustainability of their interventions.
Bridging the Gap brings these grantees together to learn from one another and inform the wider field. Each grantee is evaluating their own intervention as well as participating in a cross-site evaluation to cull lessons learned from the broader initiative. Findings from Bridging the Gap will be communicated broadly so that others can learn from our grantees’ experiences, and contribute to the national conversation about how healthcare systems can best address SDOH to improve the health of vulnerable populations.
We will use this blog to discuss issues impacting diabetes disparities, and share lessons and stories about how to Bridge the Gap. We are excited to collaborate with our grantees as we address key issues and potential solutions to reduce diabetes disparities.
(Share: Twitter) interface

